Equity Oriented Primary Care Innovation Collaborative

Racial bias and inequitable policies within the healthcare system, including primary care, have eroded the trust and use of health services over time. The COVID-19 pandemic has further exposed the increasing need to build resilient social service and primary care systems that support under-resourced communities – critical not only during a crisis but ongoing.
The Equity-Oriented Primary Care (EOPC) Innovation Collaborative is a design accelerator of geographically-distributed primary care practices and their communities working together to sustainably redesign primary care delivery to drive equitable health outcomes.
The goal of EOPC’s initial Collaborative is that by 2023, three primary care practices and their community partners will demonstrate how communities can redesign primary care services to center on racial equity.
Objectives
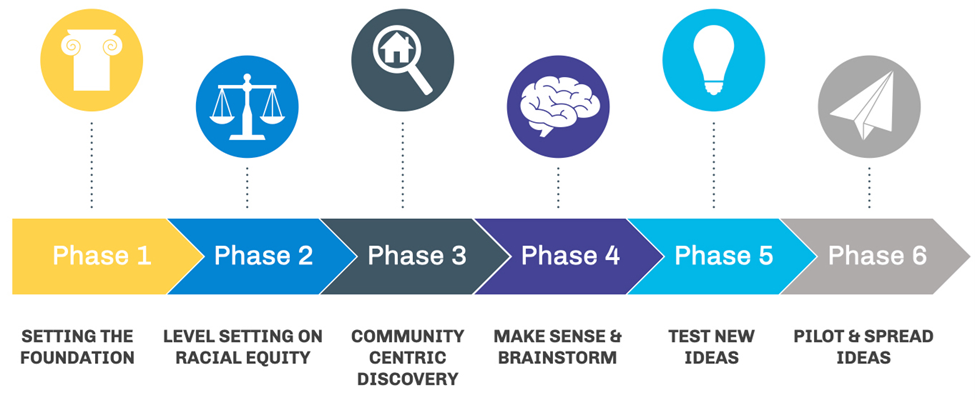
Over the course of the collaborative, each EOPC practice will use an innovation approach centered on racial and health equity to:
- Use data to reduce racial inequities in primary care practices for effective interventions.
- Co-create with communities so there is shared power and agency over their healthcare.
- Address root causes of health inequities and negative health outcomes.
- Share innovative learnings to build sustainable pilots that minimizes the effects of systemic racism and bias in primary care practices.
Focus Areas
EOPC participants will explore new or expanded solutions, and share learning structures based in innovation, community engagement, and racial healing, anchored on:
- Institutional racism and bias within primary care organizations’ policies and practices.
- Alignment of primary care strategies with community-prioritized public health efforts.
- Create sustainable financial models for new equitable care models.
Learning Questions
- How can changed policies and practices of primary care sites help reduce racial disparities in healthcare?
- How primary care can be more aligned with public health initiatives to enhance prevention strategies?
- How can we explore practical, organizational and community-centered business cases for health equity?
EOPC Participants

Matthew Walker Comprehensive Health Center, Inc. | Tennessee
Opened in 1968 as the first Federally Qualified Health Center (FQHC) in the state of Tennessee, MWCHC provides high-quality, affordable care to approximately 17,000 Middle TN residents with sites in Nashville, Clarksville, and Smyrna.

Family Medicine Practice of Karen L. Smith, MD FAAFP | North Carolina
Located in Hoke County, North Carolina, the Medicine Practice of Karen L. Smith, MD FAAP offers comprehensive services – including care coordination, preventive and behavioral health – to patients from children through adulthood.

Heartland Health Centers | Illinois
Federally-qualified health center (FQHC) with 18 locations in Chicago’s northside and suburbs. Provide comprehensive primary care, oral health and mental health services to 27,000 patients annually.
Partners with Centro Romero and local community leaders as part of the EOPC project.
Interested In Learning More?
- Check out the Rebuilding For Equity In Primary Care: Designing The Equity-Oriented Primary Care Innovation Collaborative blog post which discusses innovative strategies that other primary care practices can adapt, spread, and scale to minimize the effects of systemic inequities and racial bias.
- Watch the Applying Lessons From Costa Rica to Equity Oriented Primary Care webinar for an introduction to our Innovation Collaborative, examples on how to drive health equity in social health integration in various community health settings through a coordinated system of care, and opportunities ensure primary care, public health, and social service systems are designed to promote racial health equity.
Support This Work
For more information on investment opportunities, please contact Aziza Musa, Vice President, Business Partnerships & Investor Relations, at AMusa@healthleadsusa.org. Click here to schedule a meeting directly.
Join Us
So many organizations and individuals have resources to offer to this effort. Support our work to build collaborative, community-anchored, and equity-driven solutions that strengthen public trust and enable access to safe and effective COVID-19 vaccines.
